We have had a few patients in our clinic lately tell us they have been diagnosed as having Polycystic Ovarian Syndrome (PCOS), and when we talked to them about how they were diagnosed they told us that it was via ultrasound only.
There is far more to PCOS than cysts on the ovaries, so we thought it was time to clear the air, cut the BS (which, as you know, we love to do) and give you the facts about PCOS diagnosis.
The S in PCOS stands for SYNDROME.
If it was just about polycystic ovaries then it would be PCO. Polycystic ovaries are just one part of the picture of PCOS… not the whole part!!
The syndrome picture of PCOS means that there a range of other signs and symptoms that the patient can experience in addition to polycystic ovaries.
These include but are not limited to:
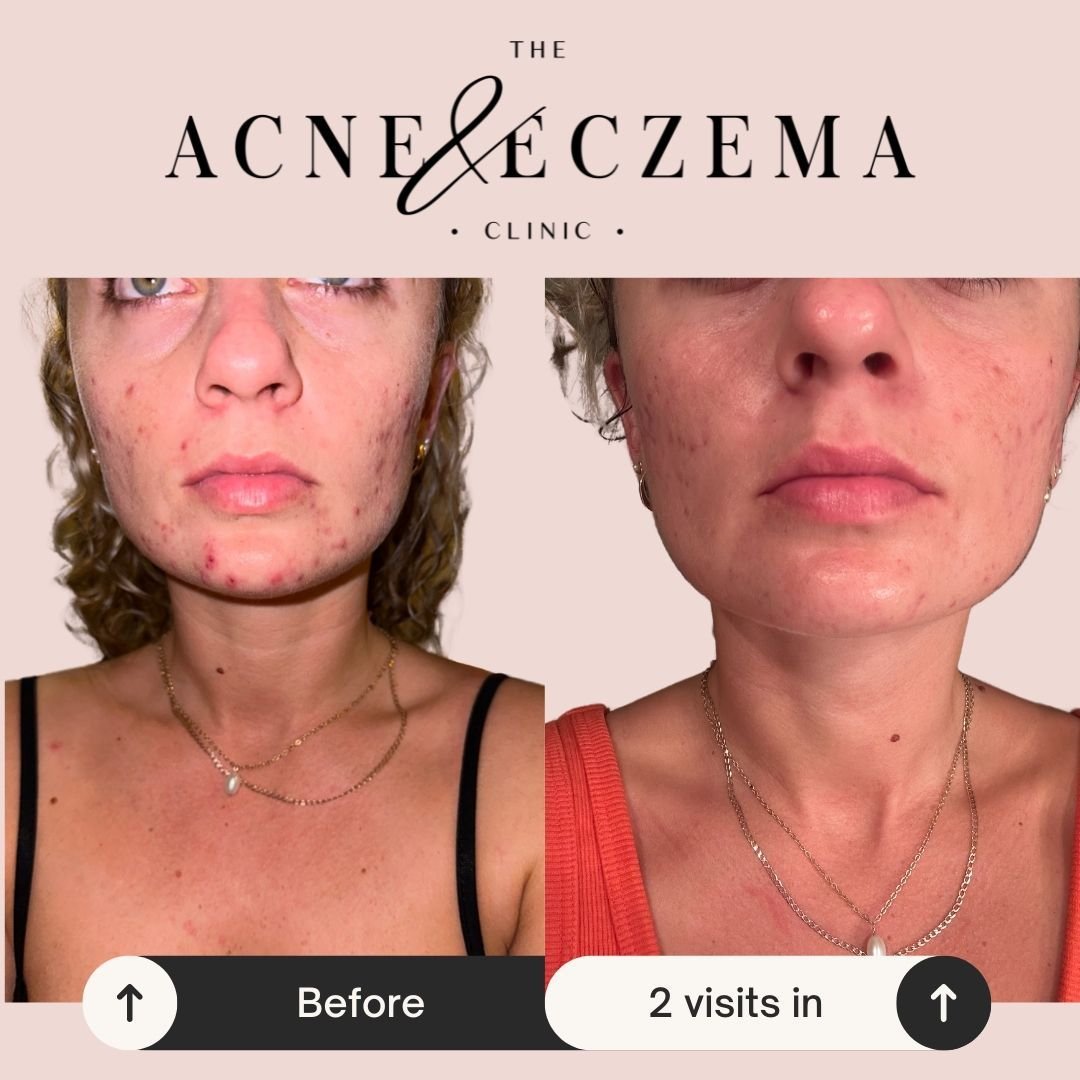
1. High androgens (testosterone is one of these), which can cause acne and increased hair growth, especially on the face, stomach and back
2. High insulin and/or blood sugar dysregulation, resulting in mood swings, weight problems and energy crashes
3. Facial hair or other excess body hair (thanks androgens!)
4. Irregular or non-existent periods
5. Abnormal menstrual bleeding patterns (usually heavy)
6. Non ovulatory menstrual cycles (this means you get a period but you haven’t ovulated)
7. Difficulty with weight (despite good nutrition and movement)
These signs and symptoms are in addition to having polycystic ovaries on ultrasound.
The fact is that not every woman with PCOS experiences all of these things… and the reality is that there has been a pretty big problem with professional bodies in the medical system reaching a systemised conclusion on what the diagnostic criteria for PCOS should be.
No surprises really, considering we are all different!
In Australia, the diagnostic criteria for PCOS is generally the Rotterdam criteria (last updated in 2011) which is used by doctors and other professionals in the medical system.
It requires that two of three of the following criteria be satisfied;
· oligo- or anovulation (inconsistent or no ovulation)
· clinical and/or biochemical hyperandrogenism (increased androgens… which requires a blood or salivary test and can not be diagnosed via ultrasound)
· polycystic ovaries on ultrasound
And here’s the “BUT, WAIT!” bit…
There are OTHER reasons that an ultrasound might show polycystic ovaries….
1. Teenagers or young adults will often have polycystic ovaries on ultrasound (up to 70%, actually) and it may take a number of years to establish a regular cycle after menarche… but this does not mean they have PCOS.
2. Being on the Oral Contraceptive Pill increases the likelihood of you having polycystic ovaries on ultrasound and once coming off the Pill (especially if you have been on it for a long time) it is common and expected to have anovulatory cycles… but this does not mean you have PCOS.
3. Once you come off the OCP you may have post pill polycystic ovaries until your cycle re establishes itself which could take a number of months… but this does not mean you have PCOS.
4. If you go on a very low carbohydrate diet and/or are not eating enough, this may both cease ovulation and show polycystic ovaries on ultrasound… but this does not mean you have PCOS.
As a side note, it’s important to recognise that the criteria has not been updated since 2011…
That’s 8 years ago and ultrasound technology is FAR better than what it was 8 years ago. Is it possible we are able to SEE more cysts than before? …Yes!
Even the Royal Australian College of General Practitioners has in their PCOS management guidelines that there should be tests performed to exclude other causes before diagnosis, such as;
· thyroid function tests
· prolactin levels
· follicle-stimulating hormone (FSH) levels
· androgen levels
In our opinion, this is just the tip of the iceberg… but the point we are making is that if you are being told that you have PCOS and that diagnosis came from an ultrasound only… without any further supporting tests… then go see someone else.
One last point to know…..
Going on the Pill will not “fix” your period or help you get a period.
The Oral Contraception Pill is a synthetic drug that essentially puts your ovaries to sleep.
You need your ovaries to be functioning properly to have normal period.
The only reason you have a bleed while you are on the Pill (when you take the sugar pill or have your week without taking it) is because of the drug withdrawal from the Pill. This is not a true menstrual bleed.
Ovulation does not occur on the Pill. When you come off the Pill the PCOS is still going to be there…
What we do differently in natural medicine is look at the whole person.
As you can see, without doing this, too many people end up being misdiagnosed!
We know how much conflicting information is out there when it comes to women’s health, and we are passionate about empowering women through education. If we knew all the ins and outs of PCOS, maybe some of us wouldn’t have been wrongly diagnosed and treated!
There are a lot of natural options for PCOS management, and we are here to help if you want to know how you can help your body naturally regulate this hormonal and metabolic condition… that’s assuming you’ve been diagnosed with the proper pathology and not just on ultrasound!
Taking the next step
If you want to explore your hormones further, then get in touch and we can discuss the best course of action for your current needs.